
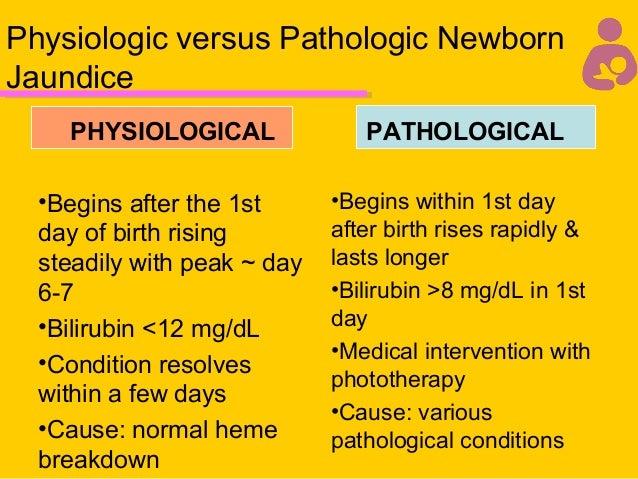
Jaundice is considered pathologic if it presents within the first 24 hours after birth, the total serum bilirubin level rises by more than 5 mg per dL (86 mol per L) per day or is higher than 17 mg per dL (290 mol per L), or an infant has signs and symptoms suggestive of serious illness. Few term newborns with hyperbilirubinemia have serious underlying pathology. Phototherapy should be instituted when the total serum bilirubin level is at or above 15 mg per dL (257 mol per L) in infants 25 to 48 hours old, 18 mg per dL (308 mol per L) in infants 49 to 72 hours old, and 20 mg per dL (342 mol per L) in infants older than 72 hours. More recent recommendations support the use of less intensive therapy in healthy term newborns with jaundice. Historically, management guidelines were derived from studies on bilirubin toxicity in infants with hemolytic disease. In the low birthweight infant, the level is proportionately lower.Hyperbilirubinemia is one of the most common problems encountered in term newborns. The specific serum level of unconjugated bilirubin that results in kernicterus is unknown, but for the term infant it has traditionally been defined as a concentration of 20 mg/dl.
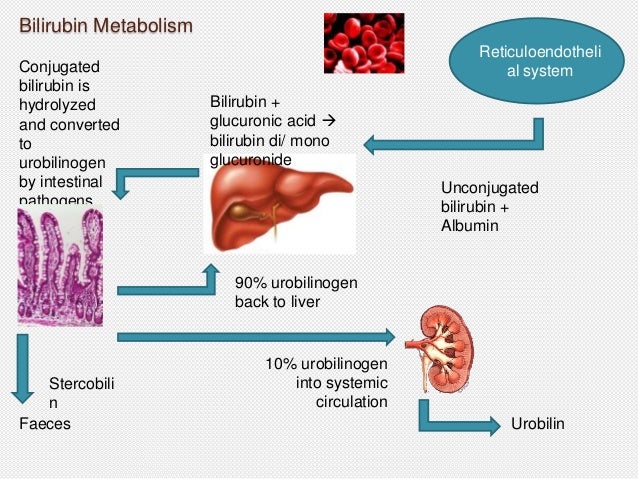
When the serum level of unconjugated bilirubin exceeds the albumin binding capacity, bilirubin diffuses into the central nervous system and may result in permanent neurological damage or death (bilirubin encephalopathy with kernicterus).Ĭonjugated bilirubin is water soluble and does not diffuse into the central nervous system so it is not capable of causing kernicterus.įactors such as acidosis and hypoalbuminemia may reduce the ability of albumin to bind to conjugated bilirubin. The level of glucuronyl transferase is initially low in the newborn and any increase in the rate of bilirubin formation can overwhelm the capacity to conjugate, thus resulting in elevated bilirubin levels. Most unconjugated bilirubin is excreted in the stool, but some is reabsorbed and returned to the liver for re-conjugation (enterohepatic circulation). In the small bowel, some of the bilirubin is hydrolyzed to yield unconjugated bilirubin and glucuronic acid. Conjugated bilirubin is secreted into the bile and enters the duodenum. Unconjugated bilirubin is bound to albumin in the plasma and transported bound to albumin to the liver and is conjugated with glucuronic acid in the hepatocytes the conjugation is catalyzed by glucuronyl transferase. Heme is catabolized to unconjugated bilirubin in the reticuloendothelial system. Excessive bruising from birth trauma or abnormal blood collections such as in a cephalohematoma may further add to the rate of RBC destruction and bilirubin formation. The rate of neonatal RBC destruction is higher than in adults resulting in greater quantity of hemoglobin release.
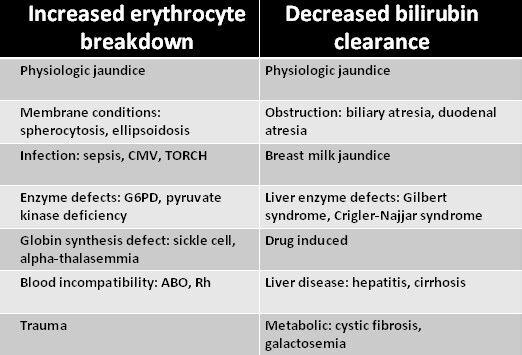
In newborns, the normal hemoglobin level is 15-18 mg/dl. Red cell hemoglobin accounts for approximately 85% of all bilirubin. Bilirubin Metabolismīilirubin is a product of heme catabolism. Although neonatal hyperbilirubinemia is usually a benign and physiologic condition, very high bilirubin levels occur in certain pathologic conditions and are potentially injurious to the central nervous system. Jaundice is seen in approximately half of all newborns.


 0 kommentar(er)
0 kommentar(er)
